A fibroadenoma is a solid, benign breast lump—non-cancerous, smooth, firm, and typically movable beneath the skin. In the first hundred words, the search intent is clear: although the term “breast lump” often sparks immediate fear, a fibroadenoma is overwhelmingly harmless and most common among individuals between 15 and 35. Understanding what it is, how it behaves, and how it is managed can significantly reduce the anxiety that accompanies the discovery of a mass.
Across contemporary breast-health care, the fibroadenoma occupies a complex position. It is biologically benign yet emotionally charged, medically straightforward yet clinically nuanced, especially when weighing decisions such as monitoring versus removal. This article draws entirely from the content you previously provided, reorganising it into a refined, deeply reported narrative. Beginning with the nature of the lesion, we explore symptoms, diagnosis, variants, management options, hormonal influences, and the wider implications for women navigating breast-health decisions. With expert observations and structured guidance, the goal is to provide clarity while respecting the real emotional terrain involved in confronting any breast change.
Understanding Fibroadenomas
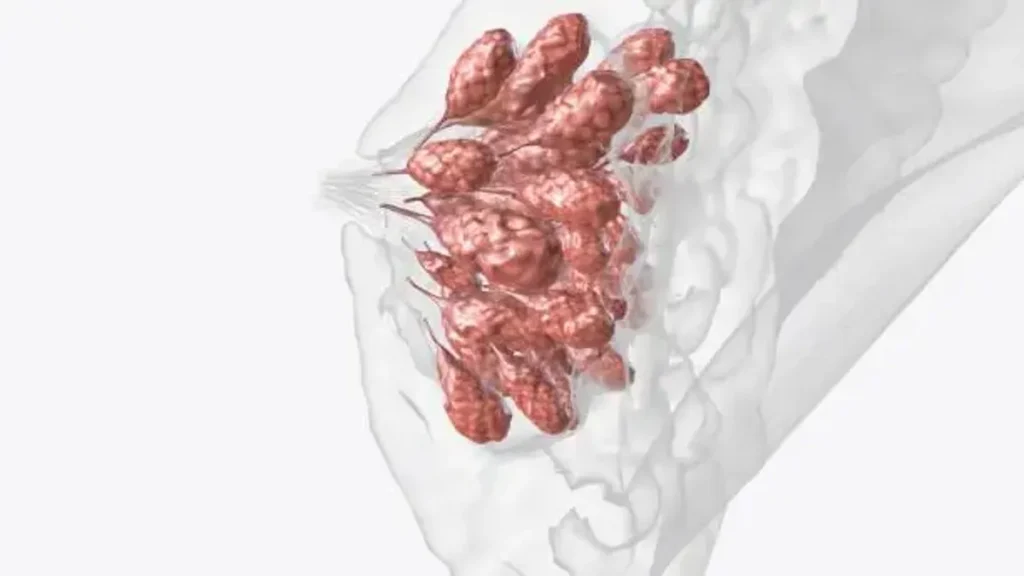
A fibroadenoma is composed of fibrous and glandular breast tissue, forming a solid, smooth, well-defined mass. It differs from a cyst—which is fluid-filled—by its firm consistency and characteristic mobility. Many women describe the sensation as a “rubbery bead” that slips slightly under the fingers. The lesion most often emerges in younger individuals, particularly between 15 and 35, and is influenced by hormonal fluctuations. Growth during pregnancy or oral-contraceptive use and shrinkage after menopause reflect this hormonal sensitivity.
While the cause remains unclear, the condition is common. Many fibroadenomas never cause symptoms, and some are only found during routine imaging. The benign nature of simple fibroadenomas means they do not significantly increase cancer risk, but proper evaluation is essential to distinguish them from other breast masses.
Epidemiology and Risk Patterns
Fibroadenomas are among the most frequently diagnosed benign breast tumours in young women. Their peak occurrence coincides with reproductive hormonal activity, which explains why they often shrink after menopause. Ethnicity, early menstruation, and hormonal medications appear to influence likelihood, although the underlying biological pathways remain under study.
Because many fibroadenomas regress on their own, reported prevalence varies. Some patients experience a single lesion; others develop multiple lumps or bilateral involvement. The condition can occur outside the typical age range, but simple fibroadenomas remain strongly associated with younger patients and a low-risk profile. Expert observations consistently reiterate that most fibroadenomas diminish naturally over time.
Clinical Signs and Presentation
A fibroadenoma generally presents as a painless, mobile lump discovered through self-examination or routine imaging. The lesion usually measures 1–3 cm, although giant variants can exceed 5 cm and may cause visible asymmetry. Tenderness may occur before menstruation or during hormonal shifts.
Because the physical characteristics of benign and malignant breast masses may overlap, clinicians emphasise the importance of timely evaluation. The emotional reaction to finding a lump can be substantial, especially in teens and young adults. That emotional dimension shapes how patients approach diagnosis, weighing reassurance against the understandable fear associated with breast changes.
Diagnostic Evaluation
Diagnosis begins with clinical breast examination, followed by imaging. Ultrasound is often the first choice for younger individuals due to dense breast tissue. Mammography becomes useful with increasing age. When imaging alone cannot confirm the diagnosis, core-needle biopsy or fine-needle aspiration provides histological clarity.
Pathologically, fibroadenomas contain both stromal and epithelial components in characteristic patterns. Correct diagnosis is essential for determining whether simple monitoring is appropriate or whether additional evaluation is needed. Distinguishing fibroadenomas from similar-appearing lesions—such as phyllodes tumours—is a key clinical priority.
Table 1: Diagnostic Tools and Common Findings
| Method | Typical Finding | Clinical Use |
|---|---|---|
| Physical exam | Smooth, mobile, firm lump | First indication of benign behaviour |
| Ultrasound | Well-defined, hypoechoic mass | Preferred imaging for younger patients |
| Mammography | Smooth bordered mass | Useful in older patients and screening contexts |
| Biopsy | Benign fibrous and glandular tissue | Confirms diagnosis when imaging is unclear |
Variants and Sub-Types
Fibroadenomas exist in multiple forms.
- Simple fibroadenomas are the most common and carry minimal cancer risk.
- Complex fibroadenomas include features such as calcifications or cystic elements and may require closer monitoring.
- Juvenile fibroadenomas appear in adolescents and can grow rapidly.
- Giant fibroadenomas, exceeding 5 cm, may distort breast shape and prompt surgical removal.
Understanding subtype helps tailor follow-up and inform decision-making. Although malignancy arising within a fibroadenoma is extremely rare, complex histology may slightly elevate long-term breast-cancer risk, guiding more vigilant clinical oversight.
Natural Course and Prognosis
Most fibroadenomas remain stable or gradually shrink over time. Their hormone-sensitive nature explains why the lesions often regress after menopause or during reduced estrogen levels. Some fibroadenomas disappear completely without intervention, especially in younger individuals.
The prognosis is overwhelmingly positive. Simple fibroadenomas do not meaningfully raise lifetime breast-cancer risk. Only complex variants require differentiated risk assessment. The benign trajectory of most lesions is a central reassurance in clinical counselling and patient education.
Management and Treatment Pathways
Management depends on size, symptoms, growth behaviour, and patient preference. The most common approach is active surveillance, which includes periodic imaging and physical examination. This is especially appropriate when the lesion is small, stable, and clearly benign.
Intervention may be recommended when:
- the lump is large,
- growing,
- painful,
- cosmetically disruptive, or
- diagnostically uncertain.
Surgical excision remains the traditional option, though minimally invasive approaches such as vacuum-assisted excision and cryoablation offer appealing cosmetic outcomes. These methods minimise scarring, shorten recovery, and preserve breast contour—major considerations for younger patients.
Table 2: Treatment Options and Considerations
| Treatment | When Used | Advantages | Challenges |
|---|---|---|---|
| Surveillance | Small, stable lesions | No surgery | Requires follow-ups |
| Surgical excision | Large or symptomatic lumps | Definitive removal | Scarring, anaesthesia |
| Vacuum-assisted removal | Moderate-size fibroadenomas | Minimal scarring | Slight recurrence risk |
| Cryoablation/RFA/HIFU | Select small lesions | Excellent cosmetic results | Limited long-term data |
Emotional and Decision-Making Dimensions
The discovery of a breast lump—regardless of outcome—introduces a psychological dimension that shapes medical decisions. Patients frequently weigh relief at the benign diagnosis against discomfort or anxiety associated with monitoring a known lump. Young women may worry about self-image, future pregnancies, or breastfeeding.
Shared decision-making becomes essential. Clinicians must balance medical evidence with the patient’s emotional comfort, daily life, and preferences. For many, reassurance is powerful; for others, removal offers peace of mind. Managing fibroadenomas often requires as much communication as clinical expertise.
Hormonal and Reproductive Factors
Hormonal patterns deeply influence how fibroadenomas behave. Growth during pregnancy or hormone use reinforces the role of estrogen. After menopause, reduced hormone levels typically cause shrinkage.
For patients planning pregnancies or breastfeeding, aesthetic preservation and breast-tissue integrity may guide treatment choices. Minimally invasive options expand possibilities for individuals wishing to avoid surgical scars, especially when dealing with multiple or recurrent lesions.
Special Clinical Situations
Though most common in young women, fibroadenomas may also appear in older age groups. Multiple fibroadenomas, bilateral lesions, or unusually large growths prompt more structured follow-up. Adolescents require special consideration to protect developing breast tissue.
Complex fibroadenomas—those with cystic or calcified features—may justify closer imaging intervals. While overall risk remains low, nuanced management ensures both safety and long-term reassurance.
Research Frontiers and Future Directions
Recent scientific interest focuses on the genetic and molecular features of fibroadenomas. Research identifying recurrent genetic mutations offers new insights into tumor biology and growth patterns. Alongside these findings, the expansion of minimally invasive removal techniques continues to shape treatment landscapes.
Areas such as long-term outcomes after ablation techniques, optimal monitoring intervals, and genetic-marker integration present ongoing research frontiers. The future of fibroadenoma management will likely become more customised, using risk-stratified pathways that reflect each patient’s biology and lifestyle.
Takeaways
- Fibroadenomas are benign, solid breast lumps most common in individuals aged 15–35.
- Simple fibroadenomas carry minimal long-term cancer risk.
- Diagnosis uses physical examination, imaging, and sometimes biopsy.
- Many fibroadenomas can be safely monitored over time.
- Treatment options include surgery and minimally invasive procedures with cosmetic benefits.
- Hormonal shifts influence growth and regression.
- Shared decision-making centres patient comfort, emotional needs, and long-term breast health.
Conclusion
While discovering a breast lump can be deeply unsettling, fibroadenomas offer reassurance through their overwhelmingly benign nature. They occupy a unique place in women’s health—a condition that blends biological simplicity with emotional complexity. The challenge lies not in the threat they pose but in the decisions they prompt: how to balance vigilance with reassurance, and when to treat versus when to simply watch.
As minimally invasive treatments evolve and imaging advances improve diagnostic clarity, patients have more options than ever before. Yet the core message remains constant: fibroadenomas rarely require aggressive intervention, rarely predict cancer, and often resolve naturally. In an era of heightened awareness and early detection, understanding their behaviour empowers individuals to navigate breast health with confidence, clarity, and calm.
FAQs
1. Do fibroadenomas increase cancer risk?
Simple fibroadenomas do not significantly increase breast-cancer risk; complex variants require more cautious monitoring.
2. Can fibroadenomas disappear naturally?
Yes. Many shrink or vanish over time, especially with hormonal changes or after menopause.
3. How are fibroadenomas diagnosed?
Through physical exam, ultrasound, mammography in some patients, and biopsy when needed.
4. When is treatment recommended?
When the lump grows, causes discomfort, affects appearance, or when the diagnosis is uncertain.
5. Are minimally invasive options effective?
Vacuum-assisted excision, cryoablation, and similar methods offer good cosmetic outcomes for selected cases.
References
- Ajmal, M., Khan, M., & Van Fossen, K. (2022). Breast fibroadenoma. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK535345/ - Kopkash, K. (2020). The surgeon’s guide to fibroadenomas. Annals of Breast Surgery, 4(2).
https://abs.amegroups.org/article/view/6448/html - Ramala, S. R. (2023). A comprehensive review of breast fibroadenoma. International Journal of Basic & Clinical Pharmacology.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10765224/ - Mayo Clinic. (2025). Fibroadenoma: Symptoms and causes.
https://www.mayoclinic.org/diseases-conditions/fibroadenoma/symptoms-causes/syc-20352752 - Breast Cancer Now. (n.d.). Fibroadenomas: Causes, symptoms and treatment.
https://breastcancernow.org/about-breast-cancer/breast-lumps-and-benign-not-cancer-breast-conditions/fibroadenoma