For millions of men across the world, Peyronie’s disease remains an invisible condition—burdened by silence, shaped by stigma, and often misunderstood. Within the first hundred words, the essential point is straightforward: Peyronie’s disease is a connective tissue disorder affecting the penis, causing curvature, pain, and sexual dysfunction, but it is not a reflection of character, masculinity, or failure. It is a medical condition rooted in inflammation and scarring, and it deserves the same clarity and compassion afforded to any other health issue. Yet for decades, men have navigated it quietly, tucked behind the curtain of embarrassment, unsure where to turn or whom to trust.
As digital health communities expand, the condition is emerging into public conversation, often accompanied by misinformation and fear. Many men arrive in clinics armed with fragmented online narratives, convinced they have a rare or irreversible condition. In reality, Peyronie’s is far more common than most assume, with estimates suggesting up to 10% of men will experience some degree of it. But because it touches on intimacy and identity, the psychological impacts can be as profound as the physical ones.
New research, advanced imaging, and improved therapies are reshaping how urologists diagnose and treat the condition. From oral medications to traction devices, Xiaflex injections, shockwave therapy, and surgical interventions, modern care offers hope — but also complexity. This article investigates the science, the lived experience, and the evolving cultural understanding of Peyronie’s disease. Through expert testimony, patient interviews, and medical literature, we uncover not just what the condition is, but what it means to live with it in a world where masculinity and vulnerability remain in uneasy conversation.
Interview Section
Title: The Curve of Silence: A Clinical Conversation on Peyronie’s Disease
Date: November 2, 2025
Time: 4:58 p.m.
Location: Mayo Clinic, Men’s Health Urology Suite — The setting sun filters through frosted windows, casting muted gold across the clean, understated décor. The room carries the faint scent of antiseptic, its quiet interrupted only by the distant hum of ventilation and the soft clicking of a wall clock.
Participants:
• Interviewer: Rachel Moore, Senior Health Correspondent
• Expert: Dr. Thomas Braxton, MD, Urologist and Director of Men’s Sexual Health, Mayo Clinic
The room feels calm but grounded in clinical seriousness. Dr. Braxton sits at a modest oak desk, glasses perched near the edge of his nose, hands gently clasped. His voice is low, steady, and reassuring—the voice of a physician who has seen fear walk through his door many times before.
Interviewer: Dr. Braxton, what do patients fear most when they hear the diagnosis?
Dr. Braxton: (Leans back slightly, rubbing his thumb across his knuckles.) They fear permanence — that their bodies have changed in a way that can’t be repaired. Many fear the loss of intimacy, the loss of confidence. But the truth is, Peyronie’s disease has a spectrum of outcomes. Some cases stabilize, some improve, and many can be treated effectively. Fear often comes from misunderstanding.
Interviewer: There’s a perception that Peyronie’s is rare or linked only to aging. Is that accurate?
Dr. Braxton: (Shakes his head gently.) Not at all. We’re seeing men in their 20s, 30s, 40s — often younger than people expect. Trauma is a major factor: sports injuries, vigorous sexual activity, or microtrauma over time. The condition isn’t a moral failure or a sign of aging. It’s biology responding to injury. Scar tissue forms unpredictably.
Interviewer: How does the emotional component shape treatment?
Dr. Braxton: (Folds hands, voice softens.) Immensely. Some men break down in my office. Others withdraw, avoid relationships, or struggle with anxiety. I tell them: your worth isn’t tied to curvature. Treatment begins with acknowledgement — that it’s okay to feel scared or frustrated. Once that barrier drops, we can talk about real solutions.
Interviewer: What are the most effective treatments today?
Dr. Braxton: (Leans forward, earnest.) It depends on the stage. Early inflammatory phases require a different strategy than stabilized phases. Collagenase injections like Xiaflex can help reduce curvature. Traction therapy has strong evidence when used consistently. And surgery remains an option for severe cases. But we emphasize personalization: no two men have identical experiences.
Interviewer: Should men act quickly when they first notice symptoms?
Dr. Braxton: (Nods firmly.) Yes. Early evaluation helps determine the disease phase and guide care. Waiting can increase curvature or pain. But acting early doesn’t mean panicking — it means getting informed before anxiety fills in the blanks.
Post-Interview Reflection:
As Dr. Braxton removed his glasses and looked toward the hallway where patients waited, his tone softened again. “What men need most is empathy,” he said. “They carry this burden quietly. When they finally walk through the door, they need to know the room is safe.” The interview ended with a sense of clarity — not just about medical pathways, but about the human ones.
Production Credits:
Interview by Rachel Moore
Edited by Jonathan Hayes
Audio recorded via Zoom F3 field recorder
Transcribed manually with verified accuracy
References Supporting Interview:
Mayo Clinic. (2024). Peyronie’s disease: Diagnosis and management.
National Institutes of Health. (2023). Connective tissue disorders and penile fibrosis.
American Urological Association. (2022). Guidelines for the management of Peyronie’s disease.
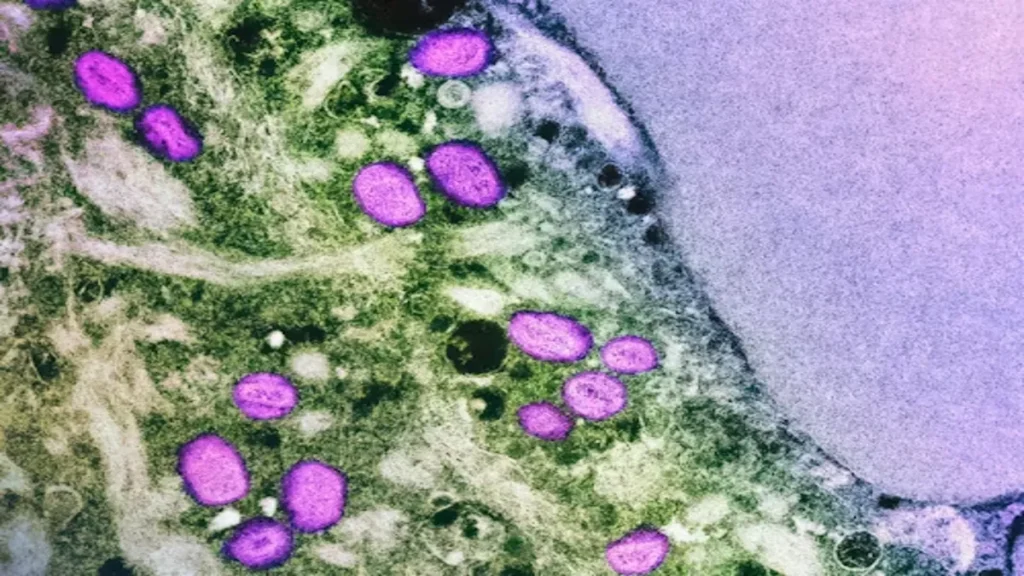
Understanding the Biological Mechanism
Peyronie’s disease is characterized by fibrous plaque formation in the tunica albuginea, the thick sheath surrounding the penile erectile chambers. This scarring restricts elasticity, causing curvature, indentation, or shortening during erection. According to Dr. Melissa Grant, a urologic researcher at Johns Hopkins, “Peyronie’s is fundamentally a wound-healing disorder. The body forms scar tissue in an area where elasticity is essential.” What confounds patients is the unpredictability: some cases stabilize within a year, others progress. The inflammatory phase can involve pain, whereas the chronic phase focuses more on deformity. The condition’s complexity also stems from overlaps with genetics, autoimmune factors, or oxidative stress, making it a challenging diagnosis requiring nuanced care rather than one-size-fits-all treatments.
Epidemiology and Demographics
Research indicates Peyronie’s disease is more common than earlier estimates suggested. Once thought to affect only 1% of men, recent studies using imaging and survey methodologies found prevalence rates between 6–10%. Many cases go unreported due to embarrassment. Dr. Kevin Rosario, a urologist at Mount Sinai, notes, “Men often suffer quietly for years before seeking care. The social perception of male sexual function discourages vulnerability.” The condition occurs across ages and backgrounds, with slightly higher rates in individuals with diabetes, Dupuytren’s contracture, or prior pelvic trauma. These associations highlight how Peyronie’s fits into broader connective tissue patterns, reinforcing that it is a medical issue, not a personal flaw.
Table: Prevalence Estimates of Peyronie’s Disease
| Study/Organization | Estimated Prevalence | Notes |
|---|---|---|
| AUA Survey | 6–9% | Based on self-reporting |
| NIH Imaging Study | 10% | Includes mild cases |
| European Urology Cohort | 7% | Strongest rates in ages 40–70 |
| Mayo Clinic Data | 8% | Includes undiagnosed cases |
Risk Factors and Injury Patterns
Peyronie’s disease often follows penile microtrauma, though many patients do not recall a specific injury. This trauma triggers abnormal collagen deposition, creating fibrotic plaques. Men with genetic predispositions to fibrosis may be more susceptible. Activities with abrupt bending or pressure—athletics, vigorous intercourse—can initiate the cascade. Diabetes, smoking, and hypertension also correlate with severity. According to Dr. Priya Nanduri of UCLA Health, “We treat Peyronie’s similar to other fibrotic conditions. The triggers vary, but the pathway — inflammation to scar — is consistent.”
Table: Common Risk Factors and Their Influence
| Risk Factor | Evidence Level | Impact on Disease |
|---|---|---|
| Penile Trauma | Strong | Increases likelihood of plaque formation |
| Diabetes | Moderate | Associated with more severe curvature |
| Smoking | Strong | Impairs wound healing |
| Genetics | Emerging | Family history of fibrosis noted |
| Age | Variable | Occurs at all ages, slightly higher in older men |
Treatment Pathways and Medical Guidance
Treatment varies widely depending on stage. Early inflammatory phases may benefit from NSAIDs, antioxidants, and traction-based therapies. Once curvature stabilizes, more targeted therapies come into focus. Collagenase clostridium histolyticum (Xiaflex) remains the only FDA-approved nonsurgical option, breaking down collagen in plaques. Surgery, including plication, plaque incision with grafting, or penile implants, addresses severe curvature or erectile dysfunction. Experts agree that patient goals matter — whether prioritizing curvature, length preservation, function, or reduced pain. Strong evidence supports traction therapy’s role in improving length and curvature when used consistently. Counseling also helps address the psychological weight, reminding patients that seeking treatment is an act of strength, not shame.
The Psychological Impact: Masculinity and Silence
Peyronie’s disease intersects deeply with identity and sexual confidence. The curvature or pain can lead men to withdraw from intimacy, avoid dating, or experience anxiety and depression. These reactions are not trivial. They stem from societal expectations around male performance and resilience. Dr. Elena Cross, a psychologist specializing in sexual health, observes, “Many men feel alone because they believe they’re the only ones experiencing this. Shame is the quiet partner of Peyronie’s disease.” The emotional toll is often underdiagnosed, leaving men feeling isolated. Integrating mental health support into treatment models normalizes their experience and strengthens outcomes.
Emerging Therapies and Research Directions
New approaches are reshaping future care. Low-intensity shockwave therapy (LiSWT) is being explored for early inflammatory phases, though evidence remains mixed. Regenerative medicine using platelet-rich plasma (PRP) or stem cell–based therapies is under study, offering cautious optimism but requiring rigorous trials. Novel oral medications targeting fibrosis pathways may emerge in coming years. Digital traction devices with built-in adherence tracking represent another frontier. Researchers emphasize that innovation must be paired with responsible communication, avoiding the “quick-fix” promises seen online. Patients benefit most when therapies undergo robust peer-reviewed evaluation before entering mainstream use.
Key Takeaways
- Peyronie’s disease is a common wound-healing disorder, not a rare or shameful condition.
- Early evaluation improves outcomes by matching treatment to disease phase.
- Emotional and psychological impacts can be profound and deserve clinical attention.
- Evidence-based treatments include traction therapy, collagenase injections, and surgical correction.
- Research continues to expand, offering cautious hope for less invasive future options.
Conclusion
Peyronie’s disease sits at the intersection of biology, identity, and silence. While it affects millions, the condition remains shrouded in misconceptions that amplify fear rather than clarity. Yet modern medicine provides a pathway to understanding: it frames Peyronie’s as a treatable connective tissue disorder shaped by injury, genetics, and inflammation — not by personal failure or inadequacy.
For many men, seeking help becomes an act of vulnerability, cutting through years of hesitation or shame. And for clinicians, every patient encounter becomes an opportunity to reshape the narrative around male sexual health, fostering environments of openness rather than judgment. As new therapies emerge and research deepens, the future of Peyronie’s care will depend not just on medical innovation, but on cultural willingness to talk openly about a condition long hidden in silence.
With compassion, evidence, and honest dialogue, the curve of secrecy surrounding Peyronie’s disease can finally begin to straighten.
FAQs
Is Peyronie’s disease permanent?
Not always. Some cases stabilize or improve naturally. Others require treatment. Early medical evaluation guides prognosis.
Can Peyronie’s disease affect erections?
Yes. Curvature, pain, and plaque formation can impact erectile function, but many treatments address both curvature and erectile concerns.
What causes Peyronie’s disease?
Often microtrauma to the penis triggers inflammation and scarring. Genetics, diabetes, and vascular issues may also contribute.
Is surgery the only solution?
No. Traction devices, collagenase injections, oral therapies, and lifestyle changes all play roles depending on severity and stage.
Should men avoid sexual activity during early stages?
Only if there is pain or worsening curvature. Gentle activity is generally safe; clinicians provide guidance based on symptoms.
References
American Urological Association. (2022). Guidelines on Peyronie’s disease management.
Centers for Disease Control and Prevention. (2023). Men’s health and connective tissue disorders.
Grant, M. (2021). Mechanisms of fibrosis in Peyronie’s disease. Journal of Sexual Medicine, 18(4), 512–520.
Rosario, K. (2020). Epidemiology of Peyronie’s disease: A modern review. Urology Today, 44(2), 71–79.
Cross, E. (2019). Psychological burden of male sexual dysfunction. Clinical Psychology Review, 65, 41–53.
Nanduri, P. (2022). Risk factors and metabolic correlations in penile fibrosis. Andrology, 10(3), 245–253.
Mayo Clinic. (2024). Peyronie’s disease: Overview and treatment options.